One of the first research programs announced under the White House BRAIN Initiative demonstrates the potential of using implanted neurotechnology to treat mental illness
Nov 30, 2018
Four years ago, DARPA announced the start of a “journey of discovery” toward understanding and treating networks of the brain. The Systems-Based Neurotechnology for Emerging Therapies (SUBNETS) program proposed to develop responsive, adaptable, closed-loop therapies for neuropsychiatric illness that incorporate recording and analysis of brain activity with near-real-time neural stimulation to correct or mitigate brain dysfunction. The premise of SUBNETS is that brain function and dysfunction — rather than being relegated to distinct anatomical regions of the brain — play out across distributed neural systems. By understanding what healthy brain activity looks like across these sub-networks, comparing that to unhealthy brain activity, and identifying predictive biomarkers that indicate changing state, DARPA plans to develop interventions that maintain a healthy brain state within a normal range of emotions.
This autumn, in three consecutive publications, researchers led by the University of California, San Francisco (UCSF) — one of two primary performers on SUBNETS, along with Massachusetts General Hospital — shared breakthroughs. First, they developed a decoding technology that can predict changes in mood from recorded neural signals. Next, they identified a specific sub-network of the brain that appears to contribute to depressed mood, especially in people with existing anxiety. Finally and most recently, they reported they were able to alleviate symptoms of moderate to severe depression using open-loop neural stimulation delivered to the orbitofrontal cortex (OFC) region of the brain to modulate a sub-network that contributes to depression. These cascading results appeared in Nature Biotechnology, Cell, and Current Biology, respectively, from September to November 2018.
Justin Sanchez, the director of DARPA’s Biological Technologies Office, oversees the SUBNETS program. Explaining the motivation behind the work, he said, “There are millions of veterans in the United States who suffer from neuropsychiatric illness, and for many of them existing treatments do not offer meaningful relief. Their experiences with mental illness have essentially been a black box against which doctors try a combination of medication and counseling, but because we have lacked a mechanistic understanding of how these illnesses manifest in the brain, these interventions are limited in their effectiveness and applicability. It is extremely frustrating for patients to not know why they feel the way they do and to not be able to correct it. We owe them and their families better options.”
DARPA’s approach was to establish if advanced neurotechnologies can offer more effective and personalized therapies that respond to an individual’s changing brain state to keep neural activity within a healthy range. Part of that work was elucidating what goes on inside the sub-networks of the brain as neuropsychiatric illnesses unfold to help doctors develop new, more effective strategies for intervention.
“The results we have demonstrated just four years into SUBNETS have validated DARPA’s approach and illuminated a path forward for developing a closed-loop system that addresses patients’ unique needs,” Sanchez said.
In the first paper, published in September, researchers from the University of Southern California (USC) described how they developed a decoding system for mood. The USC team collaborated with UCSF to collect data from volunteers among a group of epilepsy patients who already had intracranial electrodes inserted in their brains for standard clinical monitoring to locate seizures. Briefly, according to USC, “Large-scale brain signals were recorded from these electrodes in the volunteers across multiple days at UCSF, while they also intermittently reported their moods using a questionnaire. Using their methodology, the researchers were able to uncover the patterns of brain signals that matched the self-reported moods. They then used this knowledge to build a decoder that would independently recognize the patterns of signals corresponding to a certain mood. Once the decoder was built, it measured the brain signals alone to predict mood variations in each patient over multiple days.”
In early November, the UCSF team reported that they had identified localized patterns of brain activity — common across multiple volunteers — that may be responsible for feelings of low mood, particularly in people prone to anxiety. They were able to map those feelings to activity in the hippocampus and amygdala, regions of the brain that have long been linked to memory and negative emotion, respectively. Notably, that link was entirely absent from eight other research participants, all of whom had comparatively low levels of preexisting anxiety, suggesting new questions about how the brains of people prone to anxiety may differ from others in how they process emotional situations.
Most recently, UCSF announced success using open-loop stimulation of the OFC to alleviate depression. Scientists had not previously recognized the OFC as a relevant target for stimulation. In the Current Biology paper, the researchers explain how and why they selected the OFC and note, “Unilateral stimulation of the lateral OFC produced acute, dose-dependent mood state improvement in subjects with moderate-to-severe baseline depression. Behavioral responses to stimulation did not include hypomania and indicated an acute restoration to non-depressed mood state.” Stimulation of the OFC works, they proposed, because it has the effect of modulating the large-scale brain networks involved with emotional processing. Stimulation of other potential targets did not yield results that were as robust or reliable, they reported.
Stimulation of the OFC served to correct mood only in research participants who exhibited depression; it had no effect on participants who were not depressed. Further, in participants with depression, stimulation did not induce symptoms of mania, such as hyperactivity, grandiosity, or distractibility. Those patients did experience elevated speech rates, but only to levels similar to non-depressed individuals, correcting the slowed speech characteristic of individuals exhibiting depression. The researchers concluded, “These findings suggest that the effect of lateral OFC stimulation is to normalize or suppress pathological activity in circuits that mediate natural mood variation,” restoring patterns of brain activity that occurred naturally during positive moods prior to stimulation.
These findings encompass key discoveries and technologies to enable the SUBNETS goal of a closed-loop system that can detect ongoing dynamic changes in brain activity associated with fluctuations in mood, and that can use this information to deliver precisely timed therapeutic stimulation to improve brain function in individuals living with neuropsychiatric illnesses.
Sanchez anticipates that as SUBNETS begins to wind down in the coming year, results from the program will inspire additional investment and transition interest from government agencies, other partners in the White House BRAIN Initiative, and commercial industry. At the same time, DARPA will continue cooperating with the U.S. Food and Drug Administration to facilitate regulatory review of SUBNETS technologies.
“DARPA launched SUBNETS with an understanding that deep brain stimulation has the potential to treat neuropsychiatric illness, but the results of stimulation at the time were inconsistent,” Sanchez said. “What the researchers we’ve funded have been able to achieve is to begin to identify how mental illness manifests throughout the brain, and how those relevant sub-networks communicate, which starts to reveal when and where to stimulate for optimal effect. These accomplishments pave the way for additional studies that move beyond anxiety and depression, but more importantly, by demonstrating a proof of concept, they have opened the door to commercial transition so that these technologies can ultimately be put to use to improve the lives of veterans.”
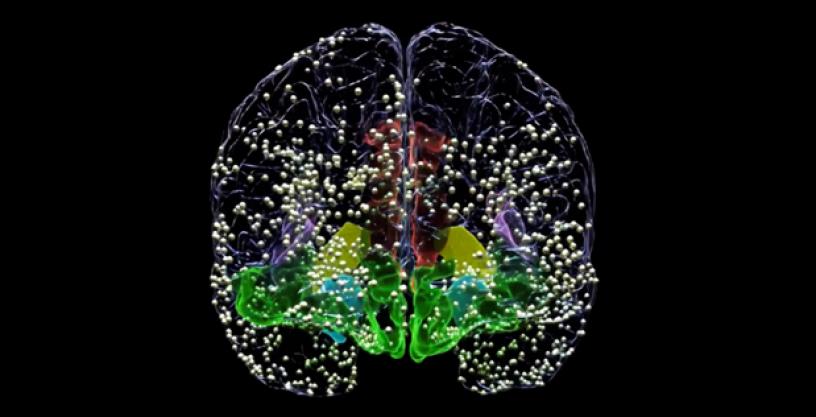
(Image Caption: This animation still illustrates the locations of all electrode recording sites used for mapping neural activity linked with natural mood fluctuations in patients awaiting surgery for epilepsy. Researchers temporarily placed electrodes in the brain for clinical seizure monitoring purposes. Each patient had a slightly different pattern of electrode placements. Credit: Chang Lab, UCSF. Animation by Ben Speidel.)
###
Media with inquiries should contact DARPA Public Affairs at outreach@darpa.mil.
Associated images posted on www.darpa.mil and video posted at www.youtube.com/darpatv may be reused according to the terms of the DARPA User Agreement, available at http://go.usa.gov/cuTXR.
